The Connection Between Addiction and Anxiety
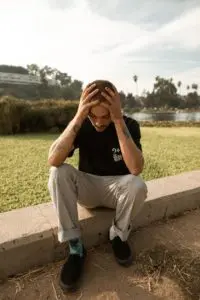 No one intends to become addicted to drugs or alcohol. Each individual has underlying factors contributing to their substance or alcohol abuse. Mood disorders such as anxiety are frequently classified as co-occurring disorders that can not only contribute to addiction but also become worse because of it.
No one intends to become addicted to drugs or alcohol. Each individual has underlying factors contributing to their substance or alcohol abuse. Mood disorders such as anxiety are frequently classified as co-occurring disorders that can not only contribute to addiction but also become worse because of it.
Addiction and Anxiety: Both Start in the Brain
The brain is a magnificent, complex communication system, and some of its capabilities have yet to be discovered. But there’s one thing neuroscientists know for sure: both addiction and anxiety originate in the brain. Why is this?
Northwestern Medicine explains that the brain’s limbic system “is responsible for the majority of emotional processing,” involving the amygdala, hippocampus, hypothalamus, and thalamus. Scientists theorize that the prefrontal cortex sends signals to prompt a person’s decision-making ability. If there’s a perceived threat, “this triggers the amygdala, which tells the hypothalamus to initiate the fight or flight response.”
The flight-or-fight response is an autonomic reaction within the body’s sympathetic nervous system that causes many types of immediate, involuntary reactions, including:
- A surge of hormones, such as cortisol and epinephrine (also referred to as adrenaline)
- Flushed skin
- Increased heart rate
- Rapid breathing
- Tensed muscles
These are also just a few of the symptoms people experience with anxiety. What’s worse, according to Harvard Health, is that chronic stress intensifies this cycle, keeping the amygdala in high-alert mode and creating even greater challenges.
So how does addiction start in and affect the brain? Yale Medicine indicates that the disease begins “when pleasure circuits in the brain get overwhelmed, in a way that can become chronic and sometimes even permanent.” A person develops substance use disorder (SUD) or alcohol use disorder (AUD) because “many drugs of abuse—such as opioids, cocaine, or nicotine—cause dopamine to flood the reward pathway, 10 times more than a natural reward.”
Then, as the brain adapts to these artificial stimuli, it becomes less tolerant, requiring more substances to achieve the same pleasurable effect. “Addiction can also cause problems with focus, memory, and learning, not to mention decision-making and judgment. Seeking drugs, therefore, is driven by habit—and not conscious, rational decisions,” Yale states.
The Cycle of Anxiety and Addiction
According to research from the National Institute on Drug Abuse, the amygdala not only retains the memory of drugs, but also triggers cravings for them. Scientists have discovered this happens regularly for anyone with SUD or AUD because of altered brain chemistry.
Findings from a 2015 study reported that “a pre-existing anxiety disorder can precipitate alcohol abuse, and high anxiety is a hallmark symptom of alcohol dependence that manifests during withdrawal. Anxiety disorders and alcohol use disorder in humans are both defined by altered amygdala structure and function, the end result of which may be disinhibition of downstream ‘effector’ regions that regulate anxiety- and alcohol-related behaviors.”
For example, research involving people who have social anxiety disorder—and approximately 15 million American adults do—indicates that many self-medicate with drugs or alcohol to try to overcome their condition. Substances with depressant effects such as alcohol or marijuana might help individuals relax and reduce inhibitions in social situations, while stimulating drugs such as cocaine, ecstasy, and methamphetamine could provide a proverbial “boost” in confidence and energy.
Anxiety.org reported study findings that identified a correlation between anxiety and substance abuse—as well as the effect of multidisciplinary treatment on relapse. “The study question was how co-occurring disorders like anxiety and depression influence relapse. In this group, 73 percent of people who were without anxiety or depression remained substance-free six months after treatment. But for people with anxiety accompanying their addiction, only 40 percent remained abstinent at the six-month point.”
So, for effective addiction treatment and recovery management, it’s not enough to simply treat the symptoms of addiction. An integrated whole-person wellness approach to healing considers not only physical health, but also emotional, mental, and even spiritual health.
How the Seabrook Model Can Help You
Some people enter addiction treatment only to discover through assessment and counseling that there are key underlying co-occuring conditions such as anxiety, depression, and others at the core of the problem.
The three phases of the Seabrook Model help address these additional factors contributing to addiction and provide a clear, structured path to long-term recovery. After detoxification, inpatient rehabilitation—based on the unique needs of each individual—focuses on healing and realignment of body, mind and spirit. The program includes comprehensive education and therapies, various wellness modalities and stress management techniques, and extensive 12-Step submersion and post-care support to ensure better health.
Our four New Jersey-based addiction treatment centers provide quality care on multiple levels. One of our admissions specialists can help determine which one is right for you or your loved one.




